Do you suffer from insomnia? Have you tried sleeping pills? When a major consumer ratings agency such as Consumer Reports endorses cognitive behavioral therapy over drug treatment for insomnia, it is big news.
In the May 2017 issue of Consumer Reports (CR), there is an article entitled Why the Best Insomnia Treatment Is Not a Drug. In earlier versions of their articles on sleep and medications for sleep they had reviewed various different sleeping agents but in this updated article they conclude that at best, the newer sleep medications add only between eight and 20 minutes of sleep time, and don’t improve how people feel or operate the next day.
They also reviewed a recent systematic research study by the federal Agency for Healthcare Research and Quality (AHRQ) that compared multiple treatments for sleep problems including drugs, cognitive behavioral therapy, and alternative therapies. This study concluded that cognitive behavioral therapy (CBT) is a safe and effective way to treat insomnia, and is more effective and safer than other treatments.
So Consumer Reports’ Best Buy drug pick is actually not a drug at all! It is Cognitive Behavioral Therapy (CBT). They recommend at least one session and optimally suggest three to six sessions of CBT with a psychologist.
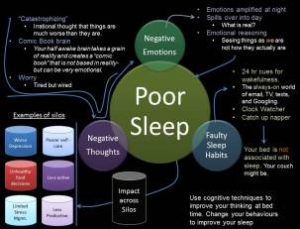
They also have a good description of how CBT works for insomnia. They explain how you meet with a psychologist and work on changing your beliefs about sleep, as well as changing certain behaviors that may contribute to insomnia. CR also includes a concise chart about bad sleep habits and how to fix them. They have an excellent description of CBT for insomnia here. If CBT was a sleep medication, promoted by a powerful drug company, it would be a multibillion-dollar product!
I have previously written about CBT for the treatment of insomnia in the article Cognitive Behavioral Therapy for Insomnia (CBT-I) Outperforms Drugs for Insomnia, Want to Sleep Better? Get Brief CBT-I Therapy for Sleep Instead of Sleeping Pills, and Good News! You May Be Getting More Sleep Than You Think, Especially If You Suffer Insomnia! so I will just summarize some of the conclusions from those articles.
The bottom line for these articles was that Cognitive Behavioral Therapy for insomnia was safe, effective and long-lasting in its effects. What is clear from virtually every study of sleep treatments is that CBT may be the only treatment for sleep problems that doesn’t have side effects and negative impacts into the next day. According to a 2015 Consumer Report survey, 36% of people who took a sleeping pill felt drowsy the next day. They also report a study of 410,000 adults published in the American Journal of Public health which found that those who took sleeping pills were twice as likely to be in automobile crashes. The researchers in this study concluded that people taking sleep medications were as likely to have car accidents as people with blood-alcohol levels above the legal limit!
So what are the recommendations and interventions used in CBT for insomnia?
- Spend only seven or eight hours in bed, and don’t compensate for insomnia by lying in bed for ten or eleven hours, as that just teaches you to be an inefficient sleeper.
- Go to bed and get up at the same time every day.
- Don’t go to bed unless you actually feel sleepy. If you can’t fall asleep get out of bed and do something peaceful and relaxing until you are sleepy, and then go back to bed.
- Try to get regular exercise but don’t exercise in the evening.
- Use your bed only for sleeping (or sex), don’t read or watch TV or look at your smartphone in bed.
- Don’t nap.
- Reduce your intake of caffeine, nicotine, and alcohol, especially later in the day.
Now it’s time for my nap—no, my mid-day exercise!